People queue for a train in Yichang, China, after the lockdowns ease.Credit: STR/AFP/Getty
A selection of the latest research on COVID-19.
1 May — Immune system shows abnormal response to COVID-19
The immune response to SARS-CoV-2 differs from the response prompted by other respiratory viruses, according to an analysis of infected cells, ferrets and people. The finding supports the idea that treatments targeting the immune system could help people with COVID-19.
Benjamin tenOever at the Icahn School of Medicine at Mount Sinai in New York City and his colleagues found that cells infected with SARS-CoV-2 produce unusually low levels of antiviral proteins called interferons compared with cells infected with other respiratory viruses (D. Blanco-Melo et al. Cell https://go.nature.com/3bWE82b, 2020). But levels of some proteins, such as IL-6, that activate more general immune responses are higher in infected ferrets and people than in uninfected controls.
The results suggest an immune imbalance: low levels of interferons reduce a cell’s ability to limit viral replication, and the activation of less-specific immune responses promotes inflammation.
30 April — Young children are not immune to COVID-19
Children are as likely as adults to become infected with SARS-CoV-2 after close contact with an infected person, according to a study of people in Shenzhen, China. Justin Lessler at Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland, Tiejian Feng at the Shenzhen Center for Disease Control and Prevention and their colleagues analysed nearly 400 cases of COVID-19 and 1,300 people who were ‘close contacts’ of the infected people (Q. Bi et al. Lancet Inf. Dis. http://doi.org/dtd7; 2020). The team found that 7% of close contacts younger than age 10 became infected — roughly the same as in the population overall. The work was first posted online as a preprint 27 March (http://doi.org/dpf9).
The researchers also found that just 9% of original cases were responsible for 80% of infections detected in close contacts. Such ‘superspreading’ events could lead to “large COVID-19 clusters”, the authors write.
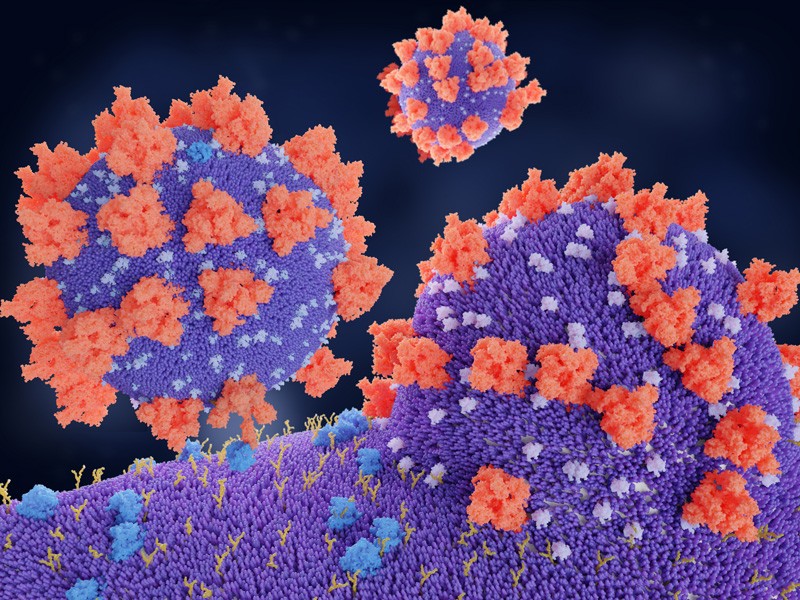
SARS-CoV-2 binds to a target cell by deploying viral proteins (red) to connect to ACE2 proteins (blue) on the target’s surface.Credit: Juan Gaertner/SPL
29 April — SARS-CoV-2 might invade by hijacking its host’s immune defences
The new coronavirus invades human cells after one of its proteins binds with ACE2, a protein found in cells in many human organs. But little has been known about that crucial interaction.
To learn more, Alex Shalek at Harvard Medical School and the Massachusetts Institute of Technology (MIT) in Boston, Jose Ordovas-Montanes at the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, and their colleagues studied airway cells from people with influenza (C. G. K. Ziegler et al. Cell http://doi.org/ds9j ; 2020). Both influenza virus and SARS-CoV-2 invade the respiratory tract.[…]
Read More: Pick of the coronavirus papers: Immune system shows abnormal response to COVID-19